Science
Our mission is to leverage FORCE data to improve outcomes for patients after the Fontan operation
Learn more about our published and in progress research below
Published Studies
Published Studies
Published Studies
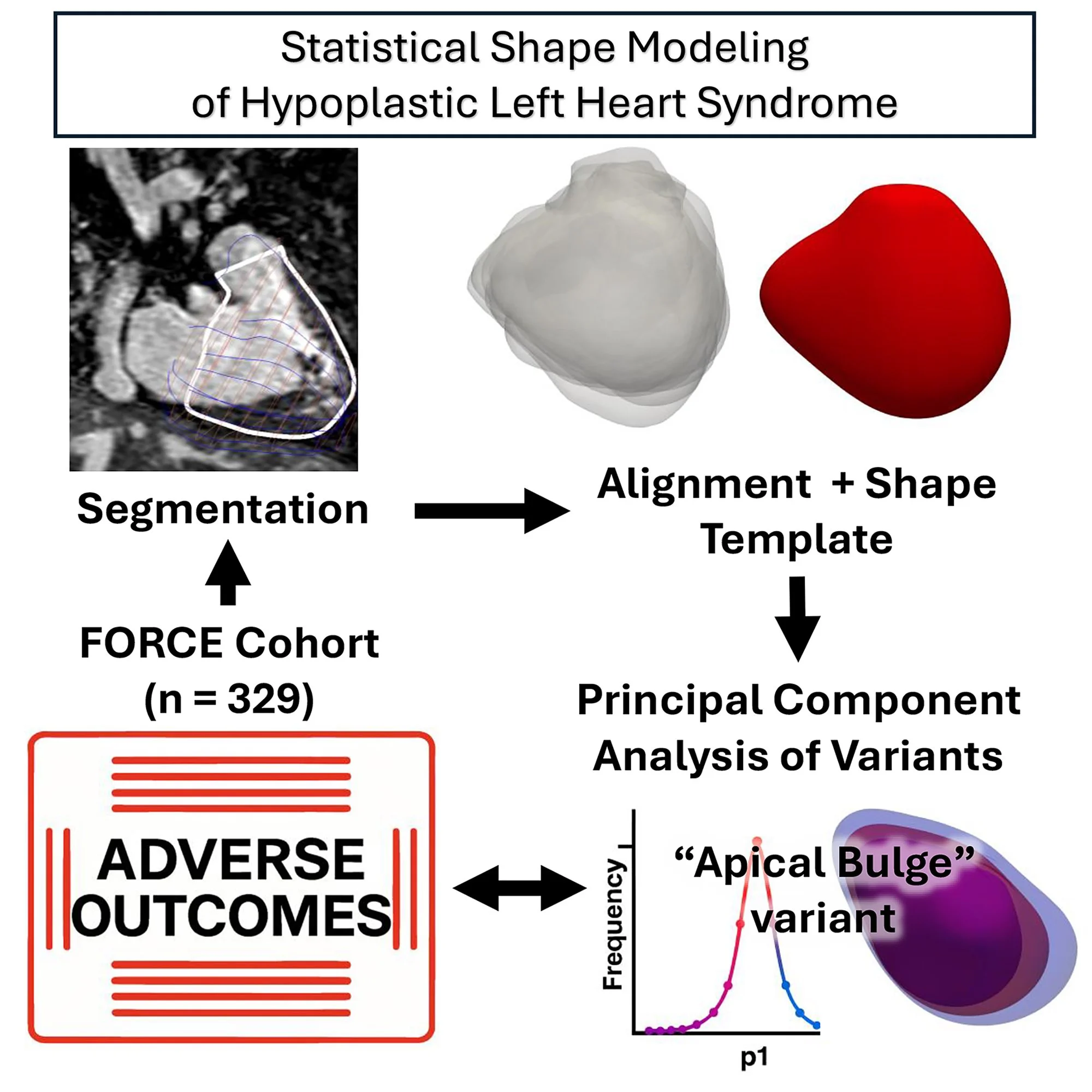
Shape Variation in Right Ventricular 3D Geometry Are Associated With Adverse Outcomes in Hypoplastic Left Heart Syndrome Patients: A Fontan Outcomes Registry Using CMR Examination (FORCE) Study
Yue-Hin Loke • Ryan O’Hara • Jacqueline Contento, • Nicole Marella, • Sarah Kollar • Ravi Vegulla, • Susana Gaviria • Rittal Mehta • Elias Balaras • Alix Fetch • Yves d’Udekem • Tarek Alsaied • Laura Olivieri • Uyen Truong • Syed Anwar • Rahul H. Rathod • Francesco Capuano • FORCE Investigators
Circulation: Cardiovascular Imaging
BACKGROUND :Assessment of the systemic right ventricle (RV) is critical for patients with hypoplastic left heart syndrome (HLHS). Traditional imaging metrics fail to capture the RV’s complex geometry and remodeling in HLHS, limiting risk stratification. We aimed to apply statistical shape modeling to a large multicenter cohort of cardiac magnetic resonance data sets to define RV shape variants and evaluate associations with clinical outcomes.
METHODS: Cardiac magnetic resonance from the FORCE (Fontan Outcomes Registry Using CMR Examinations) was analyzed for patients with HLHS post-Fontan. Three-dimensional RV models were segmented at end-diastole and processed using statistical shape modeling (ShapeWorks). Shape modes were extracted via principal component analysis and correlated with RV function, tricuspid regurgitation, remnant left ventricular morphology, and clinical outcomes, including mortality, transplant, and a composite adverse outcome including heart failure.
RESULTS:The mean RV shape template of 329 patients with HLHS (mean age, 14.7±6.3 years) depicted a circumferentially dilated RV with loss of septal concavity. RV end-diastolic volume was independently associated with composite adverse outcome (odds ratio, 6.50; P=0.001). Distinct shape modes were identified, including an apical bulge phenotype that was independently associated with composite adverse outcome (odds ratio, 2.45; P=0.047) and mortality/transplant (odds ratio, 4.24; P=0.004). This variant also correlated with RV dilation, hypertrophy, and impaired regional strain. A spheroidal shape was associated with ≥moderate tricuspid regurgitation and tricuspid annular dilation. Remnant left ventricular morphology influenced RV shape and function but not transplant-free survival.
CONCLUSIONS: Our statistical shape modeling analyses provide novel insights into RV geometric remodeling in HLHS and identify specific shape phenotypes associated with dysfunction and adverse outcomes. Shape-based metrics offer additive prognostic value beyond conventional volumetric analysis, with potential implications for risk stratification and surgical decision-making in single-ventricle physiology.
High-Performing Fontan Patients
A Fontan Outcome Registry by Cardiac Magnetic Resonance Imaging Study
Tarek Alsaied • Runjia Li • Adam B. Christopher • Mark A. Fogel • Timothy C. Slesnick • Rajesh Krishnamurthy • Vivek Muthurangu • Adam L. Dorfman • Christopher Z. Lam • Justin D. Weigand • Joshua D. Robinson • Rachael Cordina • Laura J. Olivieri • Rahul H. Rathod • FORCE Investigators
Journal of the American College of Cardiology: Advances
BACKGROUND Fontan patients exhibit decreased exercise capacity. However, there is a subset of high-performing Fontan (HPF) patients with excellent exercise capacity.
OBJECTIVES This study aims to: 1) create a Fontan-specific percent predicted peak VO2 tool using exercise data; 2) examine clinical factors associated with HPF patients; and 3) examine late outcomes in HPF patients.
METHODS Patients in the multi-institutional Fontan Outcomes Registry Using CMR Examination above the age of 8 years who had a maximal exercise test were included. An HPF patient was defined as a patient in the upper Fontanspecific percent predicted peak VO2 quartile. Multivariable logistic regression was employed to investigate factors associated with the HPF and Cox regression was used to examine the association between HPF patients and late outcomes (composite of death or listing for cardiac transplant).
RESULTS The study included 813 patients (mean age: 20.2 8.7 years). An HPF patient was associated with left ventricular morphology (OR: 1.50, P . 0.04), mixed morphology (OR: 2.23, P < 0.001), and a higher ejection fraction (OR: 1.31 for 10% increase, P . 0.01). Patients with at least moderate atrioventricular valve regurgitation, protein-losing enteropathy, or who were using psychiatric medications, were less likely to be an HPF patient. After a mean follow-up of 3.7 years, 46 (5.7%) patients developed a composite endpoint. HPF had a lower risk of death or listing for cardiac transplant (HR: 0.06 [95% CI: 0.01–0.25]).
CONCLUSIONS Patients with HPF have more favorable outcomes when compared to patients with lower exercise capacity. This large registry data highlights the role of exercise testing in providing personalized care and surveillance post-Fontan. (JACC Adv. 2024;3:101254) © 2024 The Authors. Published by Elsevier on behalf of the American College of Cardiology Foundation. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
A Deep Learning Pipeline for Assessing Ventricular Volumes from a Cardiac MRI Registry of Patients with Single Ventricle Physiology
Tina Yao • Nicole St. Clair • Gabriel F. Miller • Adam L. Dorfman • Mark A. Fogel • Sunil Ghelani • Rajesh Krishnamurthy • Christopher Z. Lam • Michael Quail • Joshua D. Robinson • David Schidlow • Timothy C. Slesnick • Justin Weigand • Jennifer A. Steeden • Rahul H. Rathod • Vivek MuthuranguMD(res)
Radiology Artificial Intelligence
Abstract: An end-to-end deep learning pipeline was developed to provide automatic segmentation and cardiac function metrics for a cardiac MRI registry of patients with single ventricle physiology; the pipeline requires no human input and is the first to segment images in this patient population.
Purpose: To develop an end-to-end deep learning (DL) pipeline for automated ventricular segmentation of cardiac MRI data from a multicenter registry of patients with Fontan circulation (Fontan Outcomes Registry Using CMR Examinations [FORCE])..
Materials and Methods: This retrospective study used 250 cardiac MRI examinations (November 2007–December 2022) from 13 institutions for training, validation, and testing. The pipeline contained three DL models: a classifier to identify short-axis cine stacks and two U-Net 3+ models for image cropping and segmentation. The automated segmentations were evaluated on the test set (n = 50) by using the Dice score. Volumetric and functional metrics derived from DL and ground truth manual segmentations were evaluated on the test set (n = 50) by using the Dice score. Volumetric and functional metrics derived from DL and ground truth manual segmentations were compared using Bland-Altman and intraclass correlation analysis. The pipeline was further qualitatively evaluated on 475 unseen examinations.ntations were compared using Bland-Altman and intraclass correlation analysis. The pipeline was further qualitatively evaluated on 475 unseen examinations.
Results: There were acceptable limits of agreement (LOA) and minimal biases between the ground truth and DL end-diastolic volume (EDV) (bias: −0.6 mL/m2, LOA: −20.6 to 19.5 mL/m2) and end-systolic volume (ESV) (bias: −1.1 mL/m2, LOA: −18.1 to 15.9 mL/m2), with high intraclass correlation coefficients (ICCs > 0.97) and Dice scores (EDV, 0.91 and ESV, 0.86). There was moderate agreement for ventricular mass (bias: −1.9 g/m2, LOA: −17.3 to 13.5 g/m2) and an ICC of 0.94. There was also acceptable agreement for stroke volume (bias: 0.6 mL/m2, LOA: −17.2 to 18.3 mL/m2) and ejection fraction (bias: 0.6%, LOA: −12.2% to 13.4%), with high ICCs (>0.81). The pipeline achieved satisfactory segmentation in 68% of the 475 unseen examinations, while 26% needed minor adjustments, 5% needed major adjustments, 5% needed major adjustments, and in 0.4%, the cropping model failed.5% needed major adjustments, and in 0.4%, the cropping model failed. and in 0.4%, the cropping model failed.
Conclusion: The DL pipeline can provide fast standardized segmentation for patients with single ventricle physiology across multiple centers. This pipeline can be applied to all cardiac MRI examinations in the FORCE registry.
Characterization and Z-score Calculation of Cardiac MRI parameters in patients after the Fontan operation. A Fontan Outcome Registry using CMR Examinations (FORCE) study
Tarek Alsaied • Runjia Li • Adam Christopher • Mark Fogel • Timothy C Slesnick • Rajesh Krishnamurthy • Vivek Muthurangu • Adam L Dorfman • Christopher Z Lam • Justin Weigand • Jong-Hyeon Jeong • Joshua D Robinson • Laura J Olivieri • Rahul H Rathod • FORCE Investigators
Journal of Cardiovascular Magnetic Resonance
Background: Cardiac magnetic resonance (CMR) offers valuable hemodynamic insights post-Fontan, but is limited by the absence of normative single ventricle data. The Fontan Outcomes Registry using CMR Examinations (FORCE) is a large international Fontan-specific CMR registry. This study used FORCE registry data to evaluate expected CMR ventricular size/function and create Fontan-specific z-scores adjusting for ventricular morphology (VM) in healthier Fontan patients.
Methods: "Healthier" Fontan patients were defined as patients free of adverse outcomes, who are New York Heart Association Class I, have mild or less valve disease, and <30% aortopulmonary collateral burden. General linear modeling was performed on 70% of the dataset to create z-scores for volumes and function. Models were tested using the remainder (30%) of the data. The z-scores were compared between children and adults. The z-scores were also compared between "healthier" Fontan and patients with adverse outcomes (death, listing for transplantation or multiorgan disease).
Results: The "healthier" Fontan population included 885 patients (15.0 ± 7.6 years) from 18 institutions with 1,156 CMR examinations. Patients with left ventricle morphology had lower volume, mass and higher ejection fraction (EF) compared to right or mixed (two-ventricles) morphology (p<0.001 for all pairwise comparisons). Gender, BSA and VM were used in z-scores. Of the "healthier" Fontan patients, 647 were children <18 years and 238 were adults. Adults had lower ascending aorta flow (2.9 ± 0.7 vs 3.3 ± 0.8L/min/m2, p<0.001) and ascending aorta flow z-scores (-0.16 ± 1.23 vs 0.05 ± 0.95, 0.02) compared to children. Additionally, there were 1595 patients with adverse outcomes who were older (16.1 ± 9.3 vs 15.0 ± 7.6, p<0.001) and less likely to have LV morphology (35 vs 47%, p<0.001). Patients with adverse outcomes had higher z-scores for ventricular volume and mass and lower z-scores for EF and ascending aorta flow compared to the "healthier" Fontan cohort.
Conclusion: This is the first study to generate CMR z-scores post-Fontan. Importantly the z-scores were generated and tested in "healthier" Fontan patients and both pediatric and adult Fontan patients. These equations may improve CMR-based risk stratification after the Fontan operation.
Cardiac MRI Predictors of Arrhythmic Sudden Cardiac Events in Patients With Fontan Circulation
Natasha K Wolfe • Mary D Schiff • Laura J Olivieri • Adam B Christopher • Mark Fogel • Timothy C Slesnick • Rajesh Krishnamurthy • Vivek Muthurangu • Adam L Dorfman • Christopher Z Lam • Justin Weigand • Joshua D Robinson • Rahul H Rathod • Tarek Alsaied • FORCE Investigators
Journal of the American College of Cardiology
Background: Among patients with congenital heart disease, those with single ventricles have the highest risk of early mortality. Sudden cardiac death is an important cause of death in this population. Understanding the risk factors for sudden cardiac events (SCE) in Fontan patients could improve prediction and prevention.
Objectives: The goal of this study was to determine the prevalence of SCE and risk factors for SCE in the Fontan population.
Methods: The Fontan Outcomes Registry Using CMR Examinations (FORCE) is an international registry collecting clinical and imaging data on Fontan patients. SCE was defined as: 1) cardiac arrest from a shockable rhythm; 2) need for emergent cardioversion/defibrillation; or 3) documented sustained ventricular tachycardia. Univariate and multivariate Cox proportional hazards regression models estimated hazard ratios for predictors of SCE.
Results: Our sample included 3,132 patients (41% female). The median age at first cardiac magnetic resonance was 14.6 years. SCE was experienced by 3.5% (n = 109) over a median follow-up time of 4.00 years. Of the 109 patients with SCE, 39 (36%) died. On multivariable analysis, NYHA functional class >II (HR: 4.91; P < 0.0001), history of protein-losing enteropathy/plastic bronchitis (HR: 2.37; P = 0.0082), single-ventricle end-diastolic volume index >104 mL/m2 (HR: 3.15; P < 0.0001), and ejection fraction <50% (HR: 1.73; P = 0.0437) were associated with SCE. Kaplan-Meier analysis demonstrated that in patients with none of the above risk factors, the 4-year freedom from SCE was 99.5%.
Conclusions: SCE occurred in 3.5% of the study population, and one-third of patients who experienced SCE died. Mild ventricular dysfunction and dilatation by cardiac magnetic resonance, NYHA functional class, and history of protein-losing enteropathy/plastic bronchitis were associated with SCE.
Increased Body Mass Index and Ventricular Cardiac Magnetic Resonance Characteristics in Adults With Fontan Circulation
Ryan D. Byrne • Stephen J. Dolgner • Christopher R. Broda • Tarek Alsaied • Mark Fogel • Timothy C. Slesnick • Rajesh Krishnamurthy • Vivek Muthurangu • Adam L. Dorfman • Christopher Z. Lam • Joshua Robinson • Rahul H. Rathod • Justin D. Weigand • FORCE Investigators
Journal of the American College of Cardiology: Advances
Background : In structurally normal hearts, increased body mass index (BMI) is associated with larger ventricular mass and volume, however, this association has yet to be described in adult Fontan patients.
Objectives: This study evaluates the relationship of increased BMI and ventricular characteristics by cardiac magnetic resonance imaging (CMR) in a multi-institutional adult Fontan population.
Methods: We conducted a multicenter, cross-sectional study using the Fontan Outcomes Registry using CMR Examinations. Fontan patients with CMR at ≥16 years of age were included. The primary independent variable was BMI and dependent variables included CMR characteristics, hemodynamics by cardiac catheterization, and clinical outcomes. Multivariable models for CMR characteristics were additionally created. Analyses were stratified by ventricular morphology.
Results: In total, 983 patients were included with 47% morphologic left ventricle (MLV) and 36% morphologic right ventricle. The median age at CMR was 21.9 years. Thirty-nine percent were overweight or obese. Increased BMI was associated with significantly higher end-diastolic volume and ventricular mass (P < 0.001 for each). In multivariable analysis, compared to normal weight, end-diastolic volume and ventricular mass were significantly elevated for obese patients (+18.0 mL; 95% CI: 8.3-27.7; P < 0.001 and + 19.1 g; 95% CI: 8.7-29.6; P < 0.001, respectively). Median ventricular end-diastolic pressure and Fontan pressure were significantly elevated with increased BMI category (P = 0.006 and P = 0.004, respectively). Stratified by ventricular morphology, similar findings were observed in MLV but not morphologic right ventricle.
Conclusions :Ventricular adaptations in volume and mass incurred by exposure to Fontan circulation are compounded by increased BMI. Obesity may disproportionately affect ventricular volume, mass, and hemodynamics in MLV
Multi-Center Comparison of Long-Term Outcomes: Extra Cardiac Conduit Fontan versus Lateral Tunnel Fontan at 15-Year Follow-Up
Laura Seese • Mary Schiff • Victor Morell • Matthew Tran • Gaurav Arora • Laura J. Olivieri • Christopher Follansbee • Adam B. Christopher • Jacqueline Kreutzer • Mark Fogel • Mario Castro Medina • Carlos E. Diaz-Castrillon • Luciana Da Fonseca Da Silva • Jose P. Da Silva • Rahul H. Rathod • Tarek Alsaied • FORCE Investigators
The Annals of Thoracic Surgery
BACKGROUND :The extracardiac conduit (ECC) and lateral tunnel (LT) are the most prevalent strategies for the Fontan operation. We utilized a multicenter database to compare long-term results.
METHODS: First-time LT or ECC Fontans performed after the year 2000 in the FORCE registry were included. Propensity score matching was employed. Outcomes were assessed individually as well as in a composite outcome that included: death, listing for transplantation, sustained atrial arrhythmias, emergent cardioversion, plastic bronchitis, protein losing enteropathy, and catheter-based intervention on the Fontan pathway. Cox proportional hazards models were used to compare hazards of outcomes between ECC and LT patients.
RESULTS: Among 3072 patients (690 LT and 1,182 ECC) in the registry, 1,290 patients (645 LT and 645 ECC) were identified after matching In matched samples, the Fontan composite outcome (32.4% vs 19.8%), sustained atrial arrhythmias (15.0% vs 5.0%), emergent cardioversion, defibrillation, or arrhythmogenic cardiac arrest (2.6% vs 0.8%), and Fontan pathway catheter-based intervention (7.1% vs 3.6%) were significantly higher for LT patients (all, p<0.05). Kaplan-Meier analysis demonstrated the 5-year, 10-year, and 15-year freedom from the composite Fontan outcome was 94.5%, 88.3%, and 79.8% for ECC patients compared to 90.2%, 80.9%, and 68.3% for LT patients (p<0.0001). ECC patients had lower hazards for atrial arrhythmia (HR=0.33, 95% CI: 0.20-0.54, p<0.0001) and the composite Fontan outcome compared to LT patients (HR=0.72, 95% CI: 0.54-0.96, p=0.0257).
CONCLUSIONS: The ECC has substantially lower hazards for atrial arrhythmias compared to the LT Fontan while other independent measures of longitudinal morbidity are similar.
The long-term effect of the Fontan fenestration on clinical outcomes: A FORCE registry study
Yu Li • Mary Schiff • Laura J. Olivieri • Adam B. Christopher • Victor Morell • Laura Seese • Rahul H. Rathod • Jacqueline Kreutzer • Tarek Alsaied • FORCE Investigators
American Heart Journal
Background : The long-term effect of open fenestration in Fontan patients is unclear, leading to wide practice variation of fenestration creation and closure. We evaluated the long-term outcomes of the fenestration using data from the Fontan Outcome Registry using Cardiac Magnetic Resonance Examinations (FORCE) Study.
Methods: Patients were categorized by fenestration status determined by post-Fontan cardiac magnetic resonance imaging (CMR) as open fenestration, nonfenestrated Fontan, spontaneous closure, and device closure. The primary outcome was the time from the CMR to the earliest event of death, listing or receiving a heart transplant, plastic bronchitis, or protein-losing enteropathy. The association between fenestration status and the outcome measure was evaluated using Cox proportional hazard models, adjusted for patients’ clinical and CMR characteristics.
Results: The cohort consisted of 2,923 patients with a median age at CMR of 14.3 years. Patients with open fenestration were younger and less likely to have a systemic left ventricle. Nonfenestrated Fontan patients were more likely to have a systemic left ventricle and lower indexed single ventricle end-diastolic volume (SVEDVi). An open fenestration was associated with adverse outcomes adjusted for clinical variables (hazard ratio 1.70, 95% CI [1.09, 2.64], P = .02). The association was no longer significant when adjusted for CMR variables, while every 10 mL/m2 increase in SVEDVi was associated with a 5% increase in the hazard of clinical outcomes (P < .0001).
Conclusion: Open fenestration is associated with adverse outcomes when adjusted for clinical characteristics. The association disappeared when additionally adjusting for CMR variables. The current practice of fenestration closure in selected patients leads to comparable outcomes with spontaneous closure and nonfenestrated Fontan.
Defining diastolic dysfunction post-Fontan: Threshold, risk factors, and associations with outcomes
Tarek Alsaied • Runjia Li • Haley Grant • Mary D. Schiff • Yu Li • Adam B. Christopher • Jacqueline Kreutzer • Bryan H. Goldstein • Jonathan H. Soslow • Yue-Hin Loke • Mark A. Fogel • Timothy C. Slesnick • Rajesh Krishnamurthy • Vivek Muthurangu • Adam L. Dorfman • Christopher Lam • Justin D. Weigand • Joshua D. Robinson • Laura J. Olivieri • Rahul H. Rathod • FORCE Investigators
American Heart Journal
Background: Following the Fontan procedure, patients with single ventricle physiology are at high risk of diastolic dysfunction (DD) and elevated end-diastolic pressure (EDP).
Objective: This study aims to determine (1) the optimal EDP threshold correlated with adverse outcomes post-Fontan and (2) the clinical and imaging predictors of DD.
Methods: The study included patients from the Fontan Outcome Registry using CMR Examinations (FORCE) who underwent cardiac catheterization and cardiac magnetic resonance (CMR) within a 2-year window. The composite outcome was defined as all-cause mortality, sustained atrial or ventricular arrhythmia, plastic bronchitis, protein-losing enteropathy, or listing for transplantation. The EDP cutoff was determined using the lowest Brier score from Cox proportional hazard models.
Results: The study included 861 patients (mean age 16.4 ± 9.3 years). Mean EDP was 9.0 ± 3.5 mm Hg, with DD defined at an optimal EDP threshold >13 mm Hg. Patients were followed for a median of 3.6 years after catheterization. By univariable analysis patients with DD were more likely to have Fontan associated liver disease (40% vs 29%, P = .03) and kidney disease (19% vs 6%, P < .001). In multivariable analyses, DD was associated with the composite outcome (HR 3.37, 95% CI: 2.03-5.59, P < .001). Ninety-seven patients (11.3%) had DD. Multivariable analysis demonstrated that older age at catheterization, greater body mass index (BMI), nonleft ventricular morphology, and higher ventricular end-diastolic volume (EDV) were associated with DD.
Conclusion: DD, defined as an EDP >13 mm Hg, is linked to over 3-fold higher risk of adverse outcomes. Risk factors for DD include older age, higher BMI, nonleft ventricular morphology, and larger EDV. The presence of risk factors may warrant screening catheterization to identify DD and modify care accordingly.
Differences in Exercise Performance in Fontan Patients with Extracardiac Conduit and Lateral Tunnel: A FORCE Fontan Registry Study
Laura Seese • Mary Schiff • Laura Olivieri • Luciana Da Fonseca Da Silva •,Jose P. Da Silva •Adam Christopher • Tyler H. Harris • Victor Morell • Mario Castro Medina • Rahul H.Rathod • Jacqueline Kreutzer • Carlos Diaz Castrillon • Melita Viegas • Tarek Alsaied • FORCE Investigators
Journal of Clinical Medicine
Background: To explore the differences in exercise capacity between the extracardiac conduit (ECC) and lateral tunnel (LT) Fontan. Methods: 2169 patients (36% LT (n = 774); 64% ECC (n = 1395)) underwent a Fontan operation between 2000 to 2023 in a multi-institutional Fontan registry. LT patients were age-matched to ECC patients, and cardiopulmonary exercise test (CPET) results were compared. Following age-matching and exclusion of those without CPET data, 470 patients emerged with 235 LT and 235 ECC patients.
Results: ECC achieved higher peak heart rates (174 vs. 169 bpm, p = 0.0008) and heart rates at ventilatory anaerobic threshold (VAT) (130 vs. 119 bpm p = 0.0005). Oxygen saturations at peak (93.0 vs. 90.0%, p = 0.0003) and baseline (95 vs. 92.5%, p < 0.0001) were higher in the ECC group. The VO2 at VAT was higher in the ECC (17.8 vs. 16.4 mL/kg/min p = 0.0123). Baseline pre-exercise heart rate, peak oxygen pulse, VE/VCO2 slope, peak VO2, peak % of predicted VO2, peak work rate, and peak % of predicted work rate were similar (all, p > 0.05). Notably, less than 35% of the cohort had a documented CPET.
Conclusions: We found that the ECC performed statistically better on many parameters of exercise capacity, including the ability to increase heart rate, have higher peak and baseline saturations, and to achieve superior VO2 at VAT. However, the magnitude of difference was small, suggesting that the translational value into the clinical realm may be limited. With a minority of the registry patients having CPET completed, this illuminates the need for the implementation of CPET surveillance for Fontan patients.